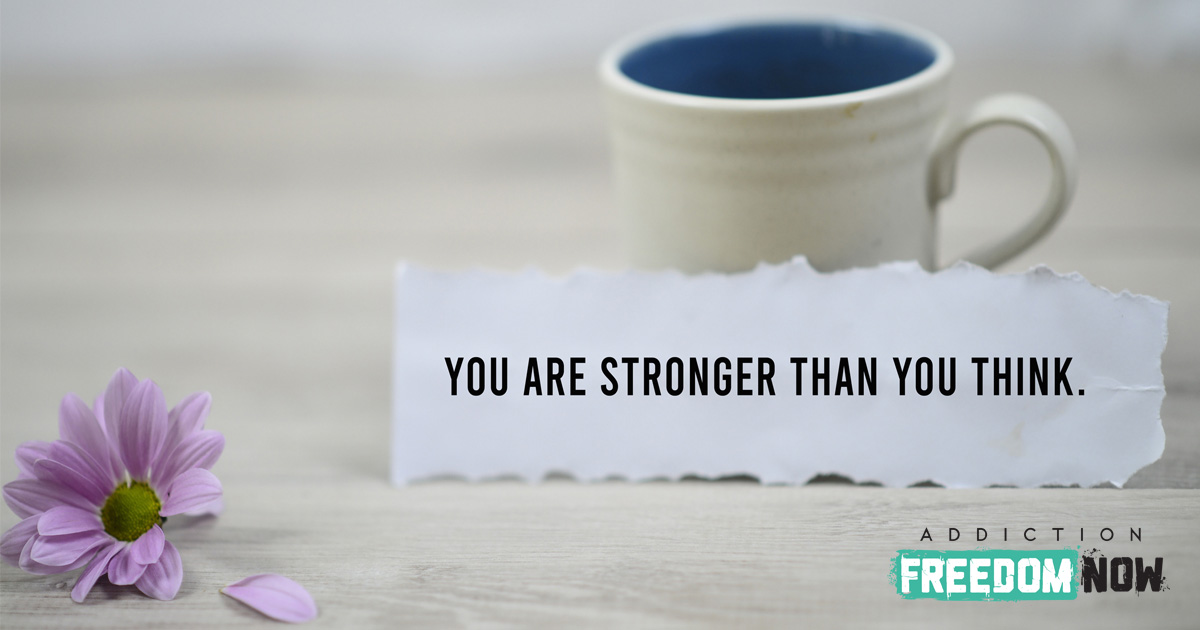
Cognitive behavioral therapy, or CBT, is a form of talk therapy used in mental health treatment to change behavior and thought patterns. It comes from the idea of behaviorism and the theory of cognition. Behaviorism is the idea that all behaviors can be conditioned, and CBT focuses on conditioning thought patterns to condition behaviors.The main goals of cognitive behavioral therapy are to help sufferers identify irrational thoughts and view them in a more logical light.
How Cognitive Behavioral Therapy Works
The main ideas of CBT are:
- Mental illnesses can be helped by correcting thoughts/ideas.
- These emotional issues are based on detrimental behavior, and
- Coping mechanisms can be taught to those suffering from mental illnesses, lessening symptoms and allowing for a healthier lifestyle.
By using CBT, therapists can address the root cause of behaviors and change thought patterns.
With this used as a tool for dependency treatment, negative patterns of thoughts can be tracked and understood more logically by allowing a patient to process their ideas and beliefs by:
- Identifying faulty logic or other bad tracks of thought and examining them more logically. This then allows a more reasonable outlook towards themselves and others
- Using this logical thought pattern to deal with various aspects of life in a healthier and more realistic way.
- Gaining a better way of viewing themselves and the people around them and gaining more confidence in their interactions with the world.
Doing so will:
- Encourage sufferers to face problems rather than participate in avoidance behavior
- Help those suffering from dependency or mental health issues talk through probable scenarios that would cause triggers or past behaviors to rise and discuss how to handle those situations.
- Help such people discover ways to be grounded and calmer so that less strain is felt on the brain and less need to revert to faulty logic and behaviors. This would lead to fewer instances of relapse.
How Does Substance Misuse Affect Cognitive Development?
People who rely on substances often get positive reinforcement through the effect of the substance, followed by the negative reinforcement of substance withdrawal. Many substances can fundamentally alter a person’s brain chemistry, and the internal need or dependence on a substance, combined with withdrawal symptoms, makes for a very difficult road. It’s a hard journey for those with substance use disorders to change their behavior, and effective treatment means fighting against many cognitive and emotional barriers.
Many don’t initially realize that mental and physical health are closely tied. The brain controls almost all the functions of the rest of the body, so when the brain is unhealthy, it affects the health of the whole body as well. Because of this, triggers are tied to both physical and mental responses. These triggers are also a good place for CBT therapists to begin intervention methods.
Triggers often include:
- High-risk scenarios, whether they are people, places, or moods.
- Negative cognitive reactions to relapse into negative behaviors, creating a cycle.
- Incorrect beliefs about substances and one’s relationship with substances.
- Thoughts, cravings, rituals, or urges that lead to the intention of using a substance.
- Justifications of negative behaviors.
How Does the Cognitive Approach Relate to Substance Use?
Because some dependencies are rooted in mental processes, particularly the faulty logic that CBT targets, this form of therapy can be very applicable and effective for substance use disorders. Those dealing with substance use disorders are fully aware that it’s unhealthy or damaging but are unable to stop using. They might not even be sure why they can’t stop misusing substances when they’re fully aware of the negative consequences.
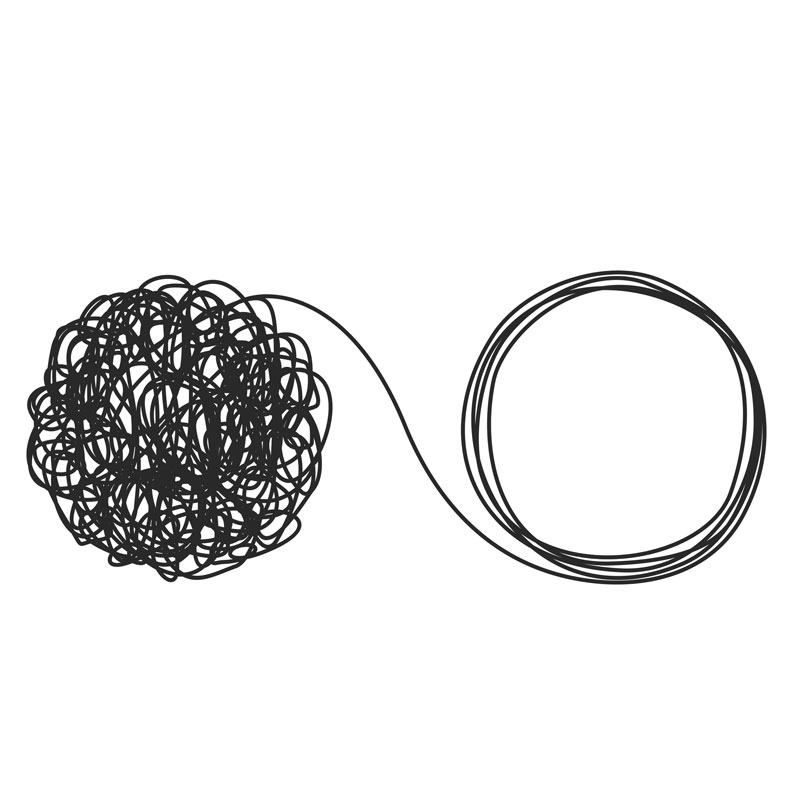
Changing this behavior is a struggle – especially when the brain is chemically addicted to a substance. By looking at substance use through the lens of CBT, the person with a substance use disorder is subject to incorrect thoughts and negative emotions, which results in their initial dependence. Often, those thoughts are connected to a mental illness, and the two disorders work in tandem to worsen the impacts of each other. These are called co-occurring disorders.
Complications of Drug and Alcohol Dependency
If someone has difficulties dealing with mental disorders, they’re more likely to turn to substance use to deal with them. A substance’s ability to change the perception of reality may be the exact draw for someone with mental illness. Though they likely know it’s unhealthy, their inaccurate thoughts may lead them to believe they’re not worth having a healthy life or that this is the only way their brain is able to function.
Co-occurring disorders are especially dangerous considering both the stigma surrounding mental illness and substance dependencies. When someone already has thoughts that make them feel less-than, the pervasive societal agreement doesn’t help. The distaste that many people hold for those suffering from these co-occurring disorders can also stop those who need treatment from seeking it out. CBT as a treatment is one of the most effective for these disorders, especially when treated together.
CBT that is focused on drug or alcohol dependency looks at a person’s thoughts and their resulting emotions, as well as the trigger events for those thoughts and emotions. Again, an attempt to find the root of the problem and to treat the faulty logic and thoughts can help prevent it from continuing to impact behavior. When someone with a substance use disorder understands what causes their dependent behavior, it’s easier for them to navigate their future. Over time, having a realistic point of view and seeing positive results from a healthier lifestyle becomes more automatic.
Can CBT Be Used for Substance Use?
Cognitive behavioral therapy uses this process of identifying negative or faulty thought patterns and understanding a more realistic thought process. CBT is a very effective treatment for the disorder since it works by changing the thoughts and behaviors that lead to substance use and introducing new coping mechanisms to deal with potential relapse triggers.
Does CBT Work for Alcoholism?
There have been numerous studies about how various forms of substance use are helped by cognitive behavior therapy. Just as with other substance use dependencies, CBT is among the most effective psychological treatment for alcoholism.
What Are the Limitations of CBT?
Studies suggest there are several barriers that could limit the effectiveness of cognitive behavior therapy. These include a lack of clinician training and certification, lack of evaluation and overarching standards, as well as lack of measurements of outcomes, lack of incentive for the implementation of CBT, lack of using evidence-based methods, and finally, the lack of supervision and monitorization. Because of each of these barriers, CBT therapy in practice may not look like the monitored versions of CBT in clinical trials and is not always widely available.
It’s important to keep in mind that a drug or alcohol dependency isn’t just mental. Once the brain has become dependent on a substance, overcoming the physical need for it may mean that those suffering from dependency need more than what CBT can offer alone.
Effectiveness of CBT for Substance Use Disorder
Cognitive behavioral therapy is very effective in the co-occurring diagnoses of mental illness and substance use disorders. The main thing that changes when treating two disorders at once rather than each separately is that a CBT therapist can help a patient understand how the two disorders contribute to and worsen each other. The end goal of CBT is always to create better coping mechanisms and a generally healthier lifestyle that doesn’t rely on a substance.
There have been many studies done on the effectiveness of CBT for substance use disorders, as well as the effectiveness of CBT on mental illness. The methods used in CBT are good for teaching coping mechanisms and cognitive skills that last long after the therapy has concluded. This allows for greater defense against triggers and subsequent relapse.